When it comes to fitting through the pelvis, head size is less important than the angle of the baby’s head.
A posterior baby will present a bigger head circumference and can sometimes get stuck in the pelvis, whereas the same baby can fit if in an anterior position. Whether or not the baby is actually too large, women may be told that a cesarean is necessary because “the baby is too big.”
When pelvic joints or the sacrum are not mobile, the pelvis won’t open to full capacity for the baby to come down. Tension or torsion in the pelvis is not that uncommon, and it can be addressed by some of the techniques on this website or by a well-trained pregnancy bodywork practitioner.
Adding mobility will make the pelvis function as if it is bigger, and allow for vaginal birth of a larger baby than would be possible if the pelvis weren’t as flexible.
There is no chart or even a realistic guideline to show which size head would fit. An ultrasound is not great at measuring fetal heads at the time of birth either. Labor itself is the key.
The pelvis opens wider during labor. The baby’s head will mold too, so a chart or a “rule” about head size is not useful.
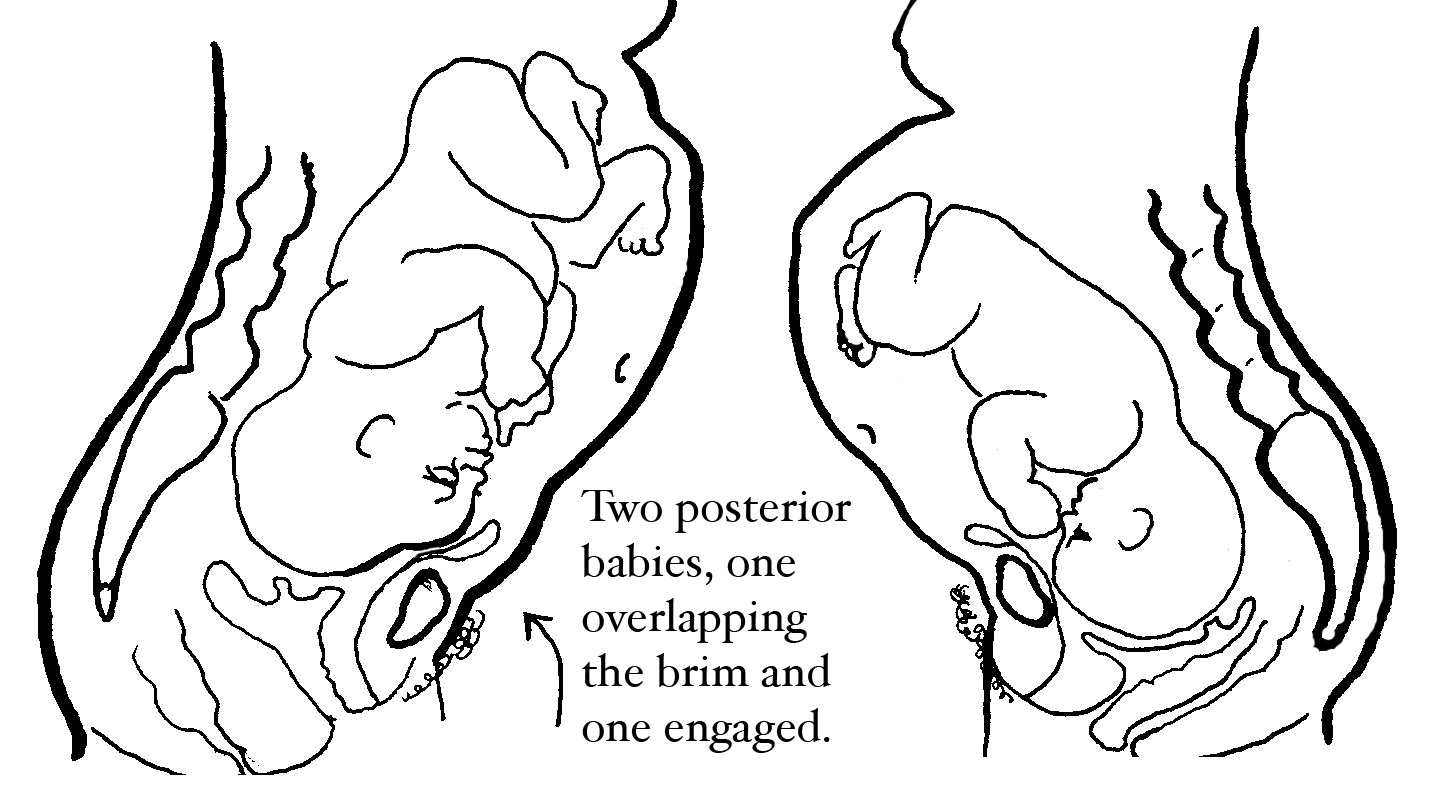
If the baby on the right can’t rotate, a cesarean will have to be performed. Whereas the baby on the left fits the mother’s pelvis, in spite of being posterior. The baby on the right needs abdominal lift and tuck for ten contractions in a row. If that doesn’t work, then do Walcher’s to open the brim.
For the uninitiated, CPD stands for Cephalopelvic Disproportion. This occurs when a baby’s head or body is too large to fit through the mother’s pelvis. It is widely believed that true CPD is rare, but many cases of “failure to progress” during labor are given a diagnosis of CPD.
How can we know if the angle of the baby’s head (either presentation or position) is stopping the birth progress and requiring a cesarean? Some posterior babies, for instance, seem too big just because the baby’s head is aimed in such a way that the head isn’t angled for an ideal birth.
To answer that question honestly, we must first support the natural physiology of birth. Freedom of movement, liberal access to food and fluids, and a calm, supportive birthing environment all work together to help labor progress normally.
When the physiology of birth is supported and the baby still doesn’t come with strong contractions, the first thing to consider is head angle, not head size. If we consider fetal rotation as a significant advance in labor progress, we might not have so many providers recommending surgery when the baby has finally rotated and the labor wanes. After rotation and a rest, labor will return—but patience is required.
After repeat cesarean, lack of progress in labor is the 2nd most common reason for cesarean delivery in the United States, accounting for 30% of nearly one million cesareans performed annually. –Gifford et al, OB Gyn Vol. 95. No. 4, April 2000
The best way to know if a baby will fit through your pelvis is to labor in vertical positions with free access to labor foods and fluids, such as hibiscus herbal tea, real grape juice, Recharge, Gatorade, Emergen-C, and other electrolyte drinks.
Women must eat over a long labor, either small amounts periodically or a full meal if desired. This can make a huge difference whether the labor is strong enough to rotate the baby’s head or not. I’m not saying that midwives should constantly bother a woman about eating though. Most mothers will tell you when they’re hungry!
Watch for the woman who hasn’t eaten well through a long latent phase, is vomiting in early labor, or whose contractions have spaced out in late labor or pushing. A lot of honey and a few grains of bee pollen, in the second stage perhaps, helps those women whose contractions aren’t strong enough on their own.
If a woman gets spacey and her contractions are spacey too, a good bowl of sweetened oatmeal is worth trying before augmenting with drugs. Oatmeal is the midwives’ Pitocin—it works great around 7 am after a long night of laboring!
Upright positions are important to help the baby rotate. There is a technique to release possible tension or torsion (twisting) in the pelvic floor: the Side-lying Release.
A birthing woman should be assisted with resting, feeding, and moving around freely during very strong labor contractions. Sadly the habit of many large, busy hospitals is to put women in bed all through labor, and often with too many drugs to labor spontaneously.
She can’t get through her labor if she doesn’t have hope. -Betty-Anne Daviss, CPM
Free movement, emotional support, and a trusting relationship with your care providers can all certainly help avoid surgical birth. Work with a doctor that you have open communication with so that when they say a cesarean is needed, you can trust them and achieve a sense of acceptance with that decision.
Latent labor is not active labor. Early labor is not active labor either. Active labor begins at about 4 cm and when the contractions are getting stronger, closer, and lasting longer. A cesarean before 4 cm should not be done for “lack of labor progress.”
In other words, a cesarean at 3 cm for “failure to progress” is entirely unjustifiable, even by ACOG standards, since active labor has not even officially begun. Hopefully, the decision to cut is not motivated by business management or—worse yet—fear management.
To confirm the diagnosis of lack of progress, ACOG recommends that women be in the active phase of labor and show no change in cervical dilatation or descent of the fetal presenting part for at least 2 hours.
A lack of progress for two or more hours does not mean the baby can’t be born vaginally and healthy, however. We simply need to address the reason(s) for the lack of progress:
The Parent Class video gives detailed instructions on avoiding unnecessary cesareans. It won’t prevent a cesarean for a truly compacted pelvis or severe scoliosis in the lumbar spine if the spine comes over the pelvic inlet, but we didn’t go from a 5% cesarean rate in 1970 to a 28% rate in 30 years because the birthing pelvis became smaller or babies got that much bigger!
I’m confident the information on this video will reduce cesareans. Download it today for comfort tonight!
Very strong contractions can happen when a posterior baby attempts to rotate to a better position to enter the pelvis. These strong contractions may not appear different from active labor.
If the baby can make the rotation to LOT, labor will often become quite manageable and less painful–even at 8 cm. This isn’t absolute after every rotation, but it does occur often. Labor can seem like the transition at 2 cm and early labor at 8 cm for these women.
Here are some more things you should know about rotation:
First, do non-pharmaceutical relaxation methods to relax the involuntary muscles. More doulas, nurses, and even physicians are using manteada (sifting) with the rebozo and craniosacral releases, such as a diaphragmatic or pelvic floor release.
If the baby hasn’t yet rotated to LOT, encourage the mother to get plenty of rest and food. Rest should include some amount of snoring, and it often takes a mature and motherly persuasion to get an anxious and exhausted birthing woman to sleep. I don’t suggest morphine, because of the risk of adding 12-24 hours of ineffective labor and possible respiratory problems for the baby after birth, even if the birth comes 24 hours later.
When rotation takes place during a long labor, rest will be needed. The contractions will begin to space out. A lull in labor doesn’t mean the baby doesn’t fit. It means the uterus is getting well-earned rest. A soothing back rub and quiet, lulling whispers may relax a mother’s mind. A nap in a pool supported with pillows, floats, rolled towels, etc. is a favorite of many women during long labors.
After 2-6 hours of good sleep or accumulated micro-naps of 2-5 minutes each (with snoring or drooling), a mother may wake, eat, and begin to move around. Contractions will resume again shortly, and more movements such as dipping in and out of squats or lunging will bring on the contractions strongly enough to bring the baby through the pelvis.
Chin tucking, whether before or after rotation, is often necessary before a vaginal birth is possible. Some posterior babies can be born vaginally even with their chins extended. (For example, read the true story, The Long Labor that Wasn’t.)
Exceptions to this would be a large pelvic outlet, a premature baby, fantastic pelvic movement and vertical positions, or vacuum extraction.
Chin tucking can take hours. Sitting on a birthing ball and making vigorous circles with your hips will reduce the time it takes. The more vigorous the circles, the faster the chin will tuck. Have someone with you and hang on to the hospital bed frame or a similar steady object so you don’t slip or wobble.
Sometimes chin tucking can happen easily, either with early labor contractions or even when a woman is asleep. Doing things that balance the body helps the baby to be flexed and ready.
A baby in an ideal laboring position can be persuaded through a well-shaped (even small) pelvis through movement and good contractions.
If the baby can’t get into a desired angle, then size might matter. Moving the pelvis and using vertical positioning, sometimes even using artificial oxytocin (Pitocin), can help when the baby is only a little big for the mom.
I’ve seen several women who were only 5 feet tall have 9, 10, and even 11-pound babies! Remember, hip size doesn’t accurately reveal the size of the inside of the pelvic “tunnel.”
Believe it or not, pelvic size changes somewhat with various maternal positions. A hands-and-knees position and squatting both open the pelvis by up to two centimeters—that’s a lot more room for a baby to use!
Squatting is especially good once the head becomes visible, even if the nurse can only see the head. Practice squatting every day in pregnancy. Just take it slow and follow the tips on the Daily Activities page.
Most babies will be rotating when their parietal bone presses down on the edge of the opening in the pelvic floor. That’s at about 5 cm for a first-time mom and not until 8 or 10 cm with moms who have given birth before.
When the baby has to rotate from the right side to the left, or the posterior to the anterior, the cervix may be at one particular dilation for 3-4 hours or more. A stall in dilation by itself is not CPD. You have to look at more indicators.
After the stall, the cervix often opens rapidly as the baby has made the change. It’s not the cervix, but rather the application of the head to the cervix and the angle of the head in the pelvis that needs addressing.
Up to 8% of babies will not rotate before delivery, whether vaginally or by cesarean. Obstetrical patients among the medical studies were able to give birth vaginally to only half of these persistent posterior babies.
Epidural anesthesia can make 12% of all babies end up in the posterior position. (See Dr. Leiberman’s 2005 study on Changes in Fetal Position)
The pelvic shape has an effect on rotation too. Two pelvic shapes in particular can sometimes limit a posterior baby’s options: the android and the anthropoid. If the baby has already dipped lower than the pelvic brim (entrance), the baby may not be able to rotate until first having descended all the way down through the pelvis and onto the perineum (which is below the lower part of the bony pelvis).
Another failure to complete rotation happens when a baby gets caught in a transverse arrest. Before or during rotation, the baby temporarily faces a hip, and in transverse arrest gets stuck there on the ischial spine halfway down the inside of the pelvis. Up to 24% of cesareans performed for “lack of progress” are done to rescue a transverse arrest baby.
There are times when a baby can’t descend because he or she doesn’t fit. There are times when even a rotated and nicely tucked baby won’t fit in the pelvis.
In these cases, try:
Natural labor contractions stop fairly abruptly–often just as the midwife is setting up her instruments, because the labor seems like transition. Or, with strong contractions, dilation remains at a standstill and there is no fetal descent and no change in chin tucking or rotation. These two seem quite opposite, but these scenarios show the two common labor patterns with CPD.
Careful vaginal exams note the relationship between the baby’s head revealing the amount of flexion (chin tucking) and whether this is changing, which often precedes descent and dilation.
Several studies show that an internal exam is only 60% accurate in the dilation stage of labor. It’s better in the pushing stage, but still only accurate 90% of the time. That means that an internal exam may not be able to distinguish the direction that the baby is facing.
Check these three things when deciding if you’ve “done everything”:
Having labor is really worth it to the baby and the breastfeeding mother. Nursing more often goes better after labor. This seems to be true in large numbers of women, even if the mother needs a cesarean to finish labor.
Midwives, both Certified Professional Midwives (usually serving home birth families and birth centers) and Certified Nurse-Midwives (working in homes, birth centers, or hospitals), have lower cesarean rates statistically than physicians — even physicians working with low-risk pregnant women. Working with a doula reduces the cesarean rate in all categories of providers as well.
Individually, a provider can help reduce a woman’s chance of cesarean whether he or she is a doctor or a midwife. It’s not the title that decides whether a woman will be pressured into a cesarean. It’s the beliefs and the skills of the person, as well as the communication and intent of the mother, her partner, and her caregivers.
A hospital nurse might have more to do with avoiding or arranging a cesarean than either the midwife or the doctor. A nurse who supports a birthing woman’s morale and knows a few fetal repositioning (rotation) tricks will help many women finish the birth themselves and avoid major surgery.
Any one of these providers might be the one to encourage a birthing woman in just the right way to finish a physiological birth when time and patience, or a series of techniques, were all that was needed for the baby to find the “hidden room” in the pelvis.
For additional education to even further enhance your pregnancy and labor preparation, shop our extensive collection of digital downloads, videos, DVDs, workbooks, and more.